- Understand the Pharmacology of Drugs Acting on the Cardiovascular System to explore anti-hypertensives, diuretics, and cardiac drugs.
- Pharmacology of Drugs Acting on the Cardiovascular System covers agents that influence heart rate, blood pressure, and vascular tone.
Shock
Pathophysiology
- Initial Stage – Compensatory mechanisms (tachycardia, vasoconstriction) maintain perfusion.
- Progressive Stage – Oxygen delivery fails → Anaerobic metabolism → Lactic acidosis → Cell dysfunction.
- Irreversible Stage – Multi-organ failure → Death if untreated.
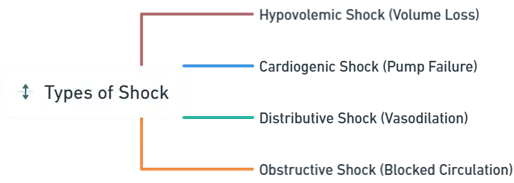
Types of Shock
-
Hypovolemic Shock (Volume Loss):
- Cause: Severe blood or fluid loss (e.g., hemorrhage, burns, diarrhea, vomiting).
- Mechanism: Reduced preload (venous return) → ↓ Stroke volume → ↓ Cardiac output.
-
Cardiogenic Shock (Pump Failure):
- Cause: Heart dysfunction (e.g., myocardial infarction, arrhythmias, myocarditis).
- Mechanism: Inability of the heart to pump blood effectively → ↓ Cardiac output.
-
Distributive Shock (Vasodilation):
- Septic Shock: Caused by severe infection and systemic inflammation.
- Anaphylactic Shock: Allergic reaction causing massive histamine release and vasodilation.
- Neurogenic Shock: Spinal cord or brain injury causing loss of vascular tone.
- Mechanism: Peripheral vasodilation → ↓ Systemic vascular resistance → Inadequate perfusion.
-
Obstructive Shock (Blocked Circulation):
- Cause: Physical obstruction (e.g., pulmonary embolism, cardiac tamponade, tension pneumothorax).
- Mechanism: Impaired blood flow → ↓ Cardiac output.
Symptoms
General Symptoms:
- Hypotension, tachycardia, cold/clammy skin (warm in distributive shock), altered mental status, oliguria, weak pulse, rapid breathing.
Specific Symptoms:
- Hypovolemic: Dry mucous membranes, reduced skin turgor, flat neck veins.
- Cardiogenic: Chest pain, lung crackles, distended neck veins.
- Septic: Early fever/flushed skin, later cool/mottled skin.
- Anaphylactic: Hives, angioedema, stridor, wheezing.
- Neurogenic: Bradycardia, warm dry skin, paralysis below injury.
Diagnosis
- Clinical Assessment: Vital signs, skin color, capillary refill.
- Laboratory Tests:
- Elevated lactate, metabolic acidosis (ABG).
- CBC, electrolytes, renal function.
- Imaging: Chest X-ray, CT, ultrasound for causes.
- Hemodynamic Monitoring: CVP, pulmonary artery catheterization.
Treatment
General Management:
- Airway: Secure airway, intubation if needed.
- Breathing: Oxygen or ventilation.
- Circulation: IV fluids, vasopressors.
Specific Treatments:
- Hypovolemic: IV crystalloids, blood transfusion if hemorrhage.
- Cardiogenic: Inotropes, diuretics, revascularization (PCI/CABG).
- Septic: Antibiotics, IV fluids, vasopressors, corticosteroids if refractory.
- Anaphylactic: IM epinephrine, antihistamines, corticosteroids, airway support.
- Neurogenic: IV fluids, vasopressors, spinal stabilization.
- Obstructive: Pericardiocentesis, chest tube, thrombolytics/embolectomy.
Prognosis and Complications
- Prognosis: Depends on type, cause, and timely intervention. Early treatment improves outcomes.
- Complications: Multi-organ dysfunction syndrome (MODS), ARDS, renal failure, death if untreated.
Thank you for reading from Firsthope's notes, don't forget to check YouTube videos!