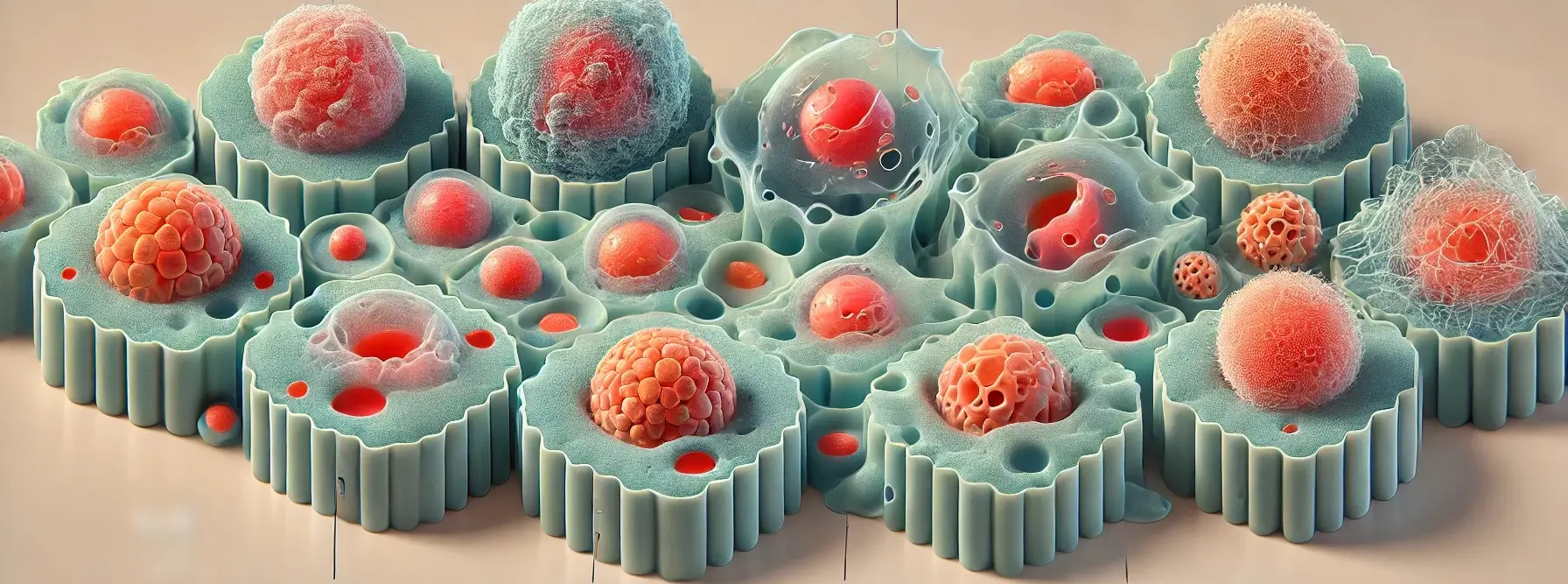
- Morphological Features of Cell Injury are structural changes in cells caused by harmful stimuli.
- In reversible injury, cells may swell, accumulate fat, and show mild organelle damage.
- In irreversible injury, more severe changes occur, such as membrane rupture and nuclear alterations like pyknosis, karyorrhexis, and karyolysis, often leading to necrosis or apoptosis.
- Morphological Features help pathologists assess the type and severity of cell damage under a microscope.
Cell Swelling
- Cell swelling, also known as hydropic change or vacuolar degeneration, is one of the earliest signs of cellular injury.
- It occurs when cells lose their ability to maintain ionic and fluid homeostasis due to damage to the plasma membrane, leading to an influx of water.
This is a sample ad placement!
-
Causes:
- Malfunction of energy-dependent ion pumps caused by hypoxia, toxins, or other disruptions to energy production.
-
Mechanism:
- ATP depletion impairs the function of membrane ion pumps, leading to sodium and water influx, which causes the cell to swell.
- Organelles like mitochondria and the endoplasmic reticulum also swell, which may disrupt cellular functions further.
-
Microscopy:
- Enlarged, pale, and turgid cells.
-
Outcome:
- Reversible if the stressor is removed; may progress to irreversible injury and cell death if persistent.
Intracellular Accumulation
- Abnormal build-up of substances within the cell, which can be endogenous (proteins, lipids, carbohydrates) or exogenous (infectious agents, minerals, pigments).
This is a sample ad placement!
-
Types of Accumulations:
- Lipids: Fatty change (steatosis) in the liver due to excessive fat deposition (e.g., from alcohol, diabetes, or obesity).
- Proteins: Accumulation of misfolded proteins (e.g., neurodegenerative diseases like Alzheimer’s).
- Pigments: Accumulation of endogenous pigments (e.g., melanin, bilirubin, lipofuscin) or exogenous pigments (e.g., carbon in anthracosis).
- Glycogen: Abnormal accumulation in glycogen storage diseases.
- Calcium: Pathological calcification, discussed below.
-
Mechanism:
- Accumulation may result from increased production, reduced degradation, or an inability to metabolize certain substances, leading to their deposition in the cytoplasm or organelles.
-
Examples:
- Fatty Change: Lipid accumulation.
- Hyaline Change: Protein accumulation.
- Hemosiderin Deposition: Iron accumulation.
-
Outcome:
- Can cause cellular dysfunction, injury, or death depending on the nature and severity of the accumulation.
Calcification
- Calcification is the abnormal deposition of calcium salts in tissues. It can be classified as dystrophic or metastatic.
This is a sample ad placement!
-
Mechanism:
- In dystrophic calcification, dead or damaged cells release intracellular contents that act as a nidus for calcium deposition.
- In metastatic calcification, elevated blood calcium levels cause calcium to be deposited in otherwise normal tissues.
-
Types:
- Dystrophic Calcification: Localized deposition in injured or dead tissues (e.g., necrotic areas, heart valves, atherosclerotic plaques), unrelated to calcium metabolism disturbances.
- Metastatic Calcification: Occurs in normal tissues due to hypercalcemia or calcium metabolism disturbances, affecting organs such as kidneys, lungs, blood vessels, and stomach.
-
Outcome:
- Impairs organ function and may lead to further tissue injury or inflammation.
Enzyme Leakage
- Enzyme leakage occurs when damaged cells, particularly those undergoing necrosis, release intracellular enzymes into the extracellular space and eventually into the bloodstream.
- These enzymes can be measured as markers of cell injury or death.
-
Mechanism:
- When the plasma membrane is damaged due to injury or cell death, cellular enzymes leak out.
- These enzymes can be detected in blood tests and are used to diagnose tissue damage.
-
Causes:
- Mechanical trauma, toxins, ischemia.
-
Clinical Relevance:
- Measurement of specific enzymes in the blood (e.g., creatine kinase for myocardial infarction, alanine aminotransferase for liver injury) helps diagnose and monitor tissue damage.
-
Outcome:
- Indicator of cell injury or death, reflecting loss of membrane integrity.
This is a sample ad placement!
Cell Death
- Cell death can occur by two main processes: necrosis and apoptosis.
Forms:
-
Apoptosis
- Necrosis is uncontrolled cell death that occurs due to severe injury, often associated with inflammation.
- It is a pathological process in which cell membranes rupture, leading to the release of cellular contents that cause inflammation in the surrounding tissue.
- Features:
- Cell shrinkage
- Chromatin condensation
- Nuclear fragmentation
- Formation of apoptotic bodies
- Phagocytosis by neighbouring or immune cells
- Outcome: Typically, does not induce an inflammatory response.
-
Necrosis
- Apoptosis is a tightly regulated, programmed cell death that is often physiological and does not elicit an inflammatory response.
- It is crucial for tissue homeostasis, development, and the elimination of damaged cells.
- Features:
- Cell swelling
- Membrane rupture
- Leakage of cellular contents
- Inflammation in surrounding tissues
- Subtypes: Coagulative necrosis and other types with distinct morphological features.
- Outcome: Final consequence of irreversible cell injury.
Thank you for reading from Firsthope's notes, don't forget to check YouTube videos!
This is a sample ad placement!