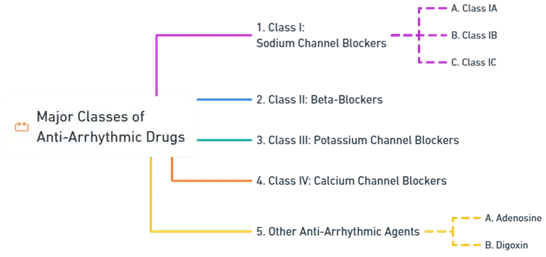
- Anti-Arrhythmic Drugs are classified based on the Vaughan-Williams classification into four main classes, each with distinct mechanisms of action.
- Learn about Anti-Arrhythmic Drugs including their classes, mechanisms, and clinical uses in treating arrhythmias effectively.
- Cardiac Arrhythmias are disturbances in the normal rhythm or rate of the heartbeat.
Major Classes of Anti-Arrhythmic Drugs:
1. Class I: Sodium Channel Blockers
- Block sodium channels, affecting phase 0 depolarization and slowing conduction velocity.
- Subclasses:
Advertisements
-
Class IA
- Examples: Quinidine, Procainamide, Disopyramide
- MOA: Block fast Na⁺ channels, prolong action potential and refractory period.
- Uses: Ventricular and supraventricular arrhythmias.
- Side Effects: Proarrhythmia (torsades de pointes), hypotension, GI disturbances.
-
Class IB
- Examples: Lidocaine, Mexiletine
- MOA: Preferentially block Na⁺ channels in ischemic/depolarized tissue, shortening action potential.
- Uses: Acute ventricular arrhythmias, post-MI.
- Side Effects: CNS effects (seizures, confusion), allergies.
-
Class IC
- Examples: Flecainide, Propafenone
- MOA: Strong Na⁺ channel blockade, slowing conduction without prolonging action potential.
- Uses: Supraventricular and ventricular arrhythmias.
- Side Effects: Proarrhythmia, bradycardia, hypotension.
Advertisements
2. Class II: Beta-Blockers
- Reduce sympathetic activity, decreasing heart rate and contractility.
- Examples: Propranolol, Metoprolol, Esmolol
- MOA: Block β-receptors, reducing AV node conduction and prolonging refractory periods.
- Uses: Supraventricular and ventricular arrhythmias, ischemic heart disease, and hypertension.
- Side Effects: Bradycardia, fatigue, bronchoconstriction.
3. Class III: Potassium Channel Blockers
- Prolong repolarization by blocking potassium channels.
- Examples: Amiodarone, Sotalol, Dofetilide
- MOA: Prolong action potential and refractory period.
- Uses: Ventricular and supraventricular arrhythmias.
- Side Effects: QT prolongation, torsades de pointes, thyroid and pulmonary toxicity (amiodarone).
Advertisements
4. Class IV: Calcium Channel Blockers
- Block calcium influx, affecting AV node conduction.
- Examples: Verapamil, Diltiazem
- MOA: Inhibit L-type Ca²⁺ channels, reducing automaticity and heart rate.
- Uses: Supraventricular arrhythmias and rate control.
- Side Effects: Bradycardia, hypotension, constipation.
5. Other Anti-Arrhythmic Agents
-
Adenosine:
- MOA: Activates A1 receptors, transient AV node blockade.
- Uses: Acute SVT termination.
- Side Effects: Transient asystole, flushing, chest discomfort.
-
Digoxin:
- MOA: Inhibits Na⁺/K⁺-ATPase, increasing vagal tone and reducing AV conduction.
- Uses: Rate control in atrial fibrillation/flutter with heart failure.
- Side Effects: Toxicity (nausea, vision changes, arrhythmias).
Clinical Considerations:
- Proarrhythmic Risks: Some anti-arrhythmics can induce new or more severe arrhythmias.
- Underlying Heart Disease: Drug choice depends on the presence of structural heart disease.
- Monitoring: Regular ECGs, electrolyte levels, and assessment for drug-specific toxicities.
Advertisements