Anti-arrhythmic drugs correct irregular heartbeats by altering cardiac impulses to restore normal rhythm and heart function.
- Anti-arrhythmic drugs are medications used to treat and prevent abnormal heart rhythms (arrhythmias).
- These drugs work by modifying the electrical activity of the heart to restore and maintain a normal heart rhythm, thereby ensuring efficient blood circulation throughout the body.
Pathophysiology of Arrhythmias
- Arrhythmias occur due to disturbances in the normal electrical conduction system of the heart. These disturbances can result from:
- Enhanced Automaticity: Increased spontaneous depolarization of cardiac cells.
- Triggered Activity: Abnormal depolarizations during or after repolarization.
- Reentrant Circuits: Circular electrical pathways that perpetuate abnormal rhythms.
- Anti-arrhythmic drugs aim to correct these disturbances by targeting various aspects of cardiac electrophysiology.
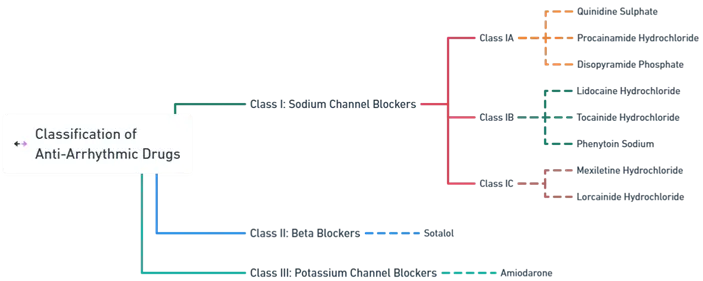
Classification of Anti-Arrhythmic Drugs
- Anti-arrhythmic drugs are primarily classified according to the Vaughan Williams Classification, which categorizes these medications based on their primary mechanism of action on cardiac cells.
Advertisements
-
Class I: Sodium Channel Blockers
-
- These drugs inhibit sodium (Na⁺) channels, reducing the rate of rise of the action potential (phase 0) in cardiac cells. They are further subdivided into:
- Class IA
- Mechanism: Moderate blockade of Na⁺ channels; also block potassium (K⁺) channels, prolonging action potential duration and refractory period.
- Drugs:
- Uses: Atrial and ventricular arrhythmias.
- Side Effects: Prolonged QT interval, torsades de pointes, hypotension.
- Class IB
- Mechanism: Mild blockade of Na⁺ channels; shorten action potential duration and refractory period.
- Drugs:
- Uses: Ventricular arrhythmias, especially post-myocardial infarction.
- Side Effects: CNS toxicity (e.g., seizures, tremors), numbness.
- Class IC
- Mechanism: Potent blockade of Na⁺ channels with minimal effect on action potential duration.
- Drugs:
- Uses: Atrial and ventricular arrhythmias.
- Side Effects: Bradycardia, hypotension, proarrhythmic effects.
-
-
Class II: Beta Blockers
-
- These drugs block beta-adrenergic receptors, decreasing the effects of sympathetic stimulation on the heart.
- Mechanism: Reduce heart rate, myocardial contractility, and conduction velocity through the atrioventricular (AV) node.
- Drugs:
- Uses: Atrial fibrillation, ventricular arrhythmias, prevention of arrhythmic recurrence.
- Side Effects: Bradycardia, hypotension, fatigue, bronchoconstriction.
-
-
Class III: Potassium Channel Blockers
- These drugs primarily block K⁺ channels, leading to prolonged repolarization and extended action potential duration.
- Mechanism: Prolong the QT interval and the refractory period without affecting Na⁺ or Ca²⁺ channels significantly.
- Drugs:
- Uses: Atrial fibrillation, ventricular tachycardia, ventricular fibrillation.
- Side Effects: Pulmonary fibrosis, thyroid dysfunction, liver toxicity, corneal deposits.
| Class | Mechanism | Drugs | Uses | Side Effects |
| Class I: Sodium Channel Blockers (IA) | Moderate Na⁺ & K⁺ blockade; prolongs action potential and refractory period | Quinidine, Procainamide, Disopyramide | Atrial and ventricular arrhythmias | Prolonged QT interval, torsades de pointes, hypotension |
| Class I: Sodium Channel Blockers (IB) | Mild Na⁺ blockade; shortens action potential duration and refractory period | Lidocaine, Phenytoin, Tocainide | Ventricular arrhythmias, especially post-MI | CNS toxicity (seizures, tremors), numbness |
| Class I: Sodium Channel Blockers (IC) | Potent Na⁺ blockade; minimal effect on action potential duration | Mexiletine, Lorcainide | Atrial and ventricular arrhythmias | Bradycardia, hypotension, proarrhythmic effects |
| Class II: Beta Blockers | Beta-adrenergic receptor blockade; reduces heart rate and AV node conduction | Sotalol | Atrial fibrillation, ventricular arrhythmias | Bradycardia, hypotension, fatigue, bronchoconstriction |
| Class III: Potassium Channel Blockers | K⁺ channel blockade; prolongs QT interval and refractory period | Amiodarone | Atrial fibrillation, ventricular tachycardia, ventricular fibrillation | Pulmonary fibrosis, thyroid dysfunction, liver toxicity, corneal deposits |