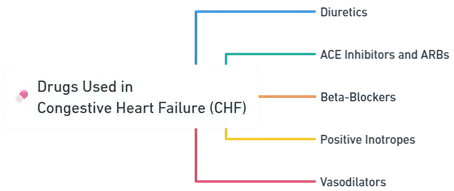
- Drugs Used in Congestive Heart Failure (CHF) include diuretics, ACE inhibitors, beta-blockers, and digitalis to improve heart function.
- Understanding Drugs Used in Congestive Heart Failure (CHF) is vital for symptom relief, slowing disease progression, and enhancing survival.
- Congestive heart failure is a clinical syndrome where the heart is unable to pump sufficient blood to meet the body’s metabolic demands.
- The main goals in pharmacotherapy are to improve hemodynamics, reduce cardiac workload, and prevent disease progression.
Major Classes of Anti-Hyperlipidemic Drugs
Advertisements
1. Diuretics
-
Mechanism of Action
- Reduce blood volume by promoting urinary excretion of sodium and water, thereby decreasing preload.
-
Common Classes
- Loop Diuretics (e.g., Furosemide): Potent diuresis by inhibiting the Na+^++-K+^++-2Cl−^-− cotransporter in the thick ascending limb of the loop of Henle.
- Thiazide Diuretics (e.g., Hydrochlorothiazide): Inhibit Na+^++-Cl−^-− cotransporter in the distal convoluted tubule.
- Potassium-Sparing Diuretics (e.g., Spironolactone): Aldosterone receptor antagonists in the collecting ducts → Prevent K+^++ loss and Na+^++ reabsorption.
-
Therapeutic Effects
- Decreased preload → Reduced pulmonary congestion and edema → Symptomatic relief.
- Spironolactone/Eplerenone also counteracts cardiac remodeling due to aldosterone.
2. ACE Inhibitors and ARBs
-
ACE Inhibitors (e.g., Enalapril, Lisinopril)
- Inhibit the angiotensin-converting enzyme, preventing formation of Angiotensin II.
- Result: Vasodilation (↓ afterload), decreased aldosterone release (↓ preload), and slowed pathologic cardiac remodeling.
-
ARBs (e.g., Losartan, Valsartan)
- Block angiotensin II type-1 receptors.
- Similar hemodynamic and protective effects to ACE inhibitors but avoid the cough side effect (caused by bradykinin accumulation in ACE inhibitors).
Advertisements
3. Beta-Blockers
-
Examples
- Carvedilol, Metoprolol, Bisoprolol.
-
Mechanism
- Inhibit excessive sympathetic drive → Decrease heart rate and contractility over the long term → Reduce oxygen demand and slow progression of HF.
- Protect against catecholamine-induced toxicity and arrhythmias.
-
Clinical Notes
- Must be started at low doses and titrated slowly due to negative inotropic effect.
- Long-term use improves survival and reduces hospitalizations.
4. Positive Inotropes
-
Digoxin
- Inhibits Na+^++-K+^++-ATPase → ↑ Intracellular Na+^++ → ↑ Intracellular Ca2+^{2+}2+ (via the Na+^++-Ca2+^{2+}2+ exchanger) → Enhanced contractility.
- Also decreases AV nodal conduction (useful for rate control in atrial fibrillation).
- Narrow therapeutic index; watch for toxicity (arrhythmias, visual changes, GI upset).
-
Other Inotropes (e.g., Dobutamine, Milrinone in acute setting)
- Dobutamine: β1_11 agonist → ↑ Contractility, modest ↑ HR.
- Milrinone: Phosphodiesterase-3 inhibitor → ↑ cAMP → ↑ Ca2+^{2+}2+ influx → Positive inotropy and vasodilation.
Advertisements
5. Vasodilators
-
Hydralazine + Isosorbide Dinitrate
- Hydralazine: Arteriolar dilator → ↓ Afterload.
- Isosorbide Dinitrate: Venodilator → ↓ Preload.
- Particularly beneficial in certain patient populations (e.g., African American patients with HF).
Clinical Considerations:
- Combination Therapy: Often necessary for optimal management.
- Monitoring: Regular assessment of renal function, electrolytes, and heart function.
- Individualization: Tailoring therapy based on patient-specific factors.
Click Here to Watch the Best Pharma Videos
Advertisements