- This article explains the Drugs Used in the Therapy of Shock such as vasopressors, inotropes, and fluids for emergency care.
- Drugs Used in the Therapy of Shock help restore blood pressure, perfusion, and organ function in critical conditions.
- Shock is a critical condition characterized by inadequate tissue perfusion and oxygenation, leading to cellular dysfunction and potential organ failure.
- Pharmacological management aims to restore adequate circulation and oxygen delivery.
- Shock can be classified into several types, each requiring specific therapeutic agents:
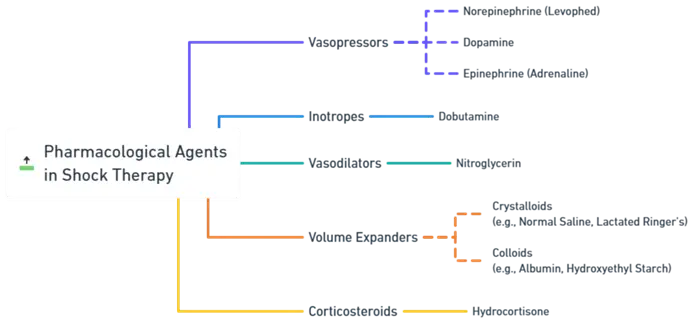
Pharmacological Agents in Shock Therapy:
Advertisements
1. Vasopressors:
-
Norepinephrine (Levophed):
- Mechanism: Primarily alpha-adrenergic agonist with some beta-1 activity, causing vasoconstriction and increased cardiac contractility.
- Use: First-line agent in septic shock; helps increase blood pressure and improve perfusion.
- Side Effects: Arrhythmias, excessive vasoconstriction leading to peripheral ischemia.
-
Dopamine:
- Mechanism: Dose-dependent effects:
- Low doses: Dopaminergic receptors, causing renal vasodilation.
- Intermediate doses: Beta-1 adrenergic effects, increasing heart rate and contractility.
- High doses: Alpha-adrenergic effects, causing vasoconstriction.
- Use: Cardiogenic and hypovolemic shock; aims to improve cardiac output and blood pressure.
- Side Effects: Tachycardia, arrhythmias, ischemia at high doses.
- Mechanism: Dose-dependent effects:
-
Epinephrine (Adrenaline):
- Mechanism: Non-selective adrenergic agonist affecting alpha and beta receptors; increases heart rate, contractility, and causes vasoconstriction.
- Use: Anaphylactic shock, cardiac arrest; sometimes used in septic shock.
- Side Effects: Tachycardia, arrhythmias, increased myocardial oxygen demand.
2. Inotropes:
-
Dobutamine:
- Mechanism: Primarily beta-1 adrenergic agonist, increasing cardiac contractility and output with mild vasodilation.
- Use: Cardiogenic shock; improves heart performance.
- Side Effects: Arrhythmias, hypotension.
Advertisements
3. Vasodilators:
-
Nitroglycerin:
- Mechanism: Nitric oxide donor causing vasodilation, particularly in veins and coronary arteries.
- Use: Initially in hypertensive emergencies or specific types of shock (e.g., cardiogenic shock due to myocardial infarction).
- Side Effects: Hypotension, headache, reflex tachycardia.
4. Volume Expanders:
-
Crystalloids (e.g., Normal Saline, Lactated Ringer’s):
- Mechanism: Restore intravascular volume through isotonic solutions.
- Use: Hypovolemic shock due to fluid loss.
- Side Effects: Fluid overload, electrolyte imbalances.
-
Colloids (e.g., Albumin, Hydroxyethyl Starch):
- Mechanism: Larger molecules remain in the intravascular space longer, providing sustained volume expansion.
- Use: Similar to crystalloids but when longer-lasting volume expansion is needed.
- Side Effects: Allergic reactions, coagulopathy with some colloids.
Advertisements
5. Corticosteroids:
-
Hydrocortisone:
- Mechanism: Anti-inflammatory effects; may help in septic shock by enhancing vascular responsiveness to vasopressors.
- Use: Septic shock unresponsive to fluid and vasopressor therapy.
- Side Effects: Immunosuppression, hyperglycemia, electrolyte disturbances.
Clinical Considerations:
- Hemodynamic Monitoring: Essential to guide therapy, including blood pressure, heart rate, central venous pressure, and cardiac output.
- Etiology-Specific Treatment: Address the underlying cause (e.g., antibiotics in septic shock, fluids in hypovolemic shock).
- Balanced Approach: Avoid overuse of vasopressors which can lead to tissue ischemia; combine with appropriate fluid management.
Click Here to Watch the Best Pharma Videos
Advertisements