Tissue Permeability of Drugs depends on lipid solubility, ionization, molecular size, and membrane transport mechanisms.
- Tissue permeability refers to the ability of drugs to cross cell membranes and enter tissues, influencing drug distribution and therapeutic action.
- It depends on both drug properties and physiological barriers.
Advertisements
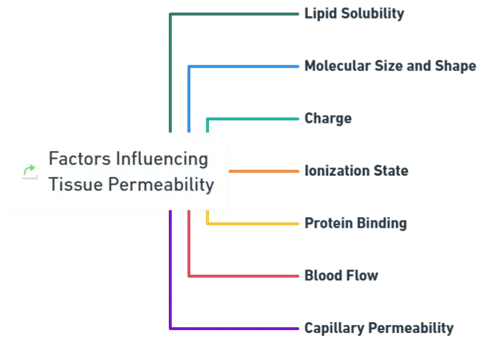
Factors Influencing Tissue Permeability
-
Lipid Solubility
- Lipid-soluble drugs easily diffuse through the lipid bilayer of cell membranes.
- Water-soluble drugs require transporters or channels to cross membranes.
-
Molecular Size and Shape
- Smaller, more compact molecules pass through membranes more easily than larger, bulkier ones.
-
Charge
- Charged molecules may need specific transporters or channels, while uncharged molecules can diffuse more readily.
-
Ionization State
- The pH of the surrounding environment influences a drug’s ionization, affecting its ability to cross membranes.
- Acidic drugs tend to accumulate in acidic tissues (e.g., stomach), while basic drugs accumulate in basic tissues (e.g., liver).
-
Protein Binding
- Many drugs bind to plasma proteins (e.g., albumin), reducing their availability for tissue distribution.
- Only unbound (free) drugs are available for active transport into tissues.
-
Blood Flow
- Highly perfused organs (e.g., liver, kidneys, brain) receive drugs more rapidly than low-perfusion tissues (e.g., adipose tissue).
-
Capillary Permeability
- The permeability of capillaries influences how easily drugs enter tissues.
- Some tissues, such as the brain, have highly selective barriers, while others, like the liver, allow easier drug passage.
Advertisements