- Tuberculosis is a potentially severe infectious disease primarily affecting the lungs (pulmonary TB) but can also affect other parts of the body (extrapulmonary TB).
- It is caused by the bacterium Mycobacterium tuberculosis.
Signs and Symptoms of Tuberculosis
-
Pulmonary TB:
- Persistent Cough: Lasting more than three weeks, sometimes producing blood (hemoptysis).
- Chest Pain: Painful breathing or coughing.
- Fever and Chills: Often in the evening.
- Night Sweats: Profuse sweating at night.
- Weight Loss: Unintended weight loss and loss of appetite.
- Fatigue: Persistent tiredness and weakness.
-
Extrapulmonary TB:
- Lymphadenitis: Swollen lymph nodes.
- Meningitis: TB infection of the brain lining, causing headaches, fever, and neurological symptoms.
- Skeletal TB: Affects bones and joints, leading to pain and swelling.
- Genitourinary TB: Involving kidneys, bladder, or reproductive organs.
- Miliary TB: Disseminated TB affecting multiple organs.
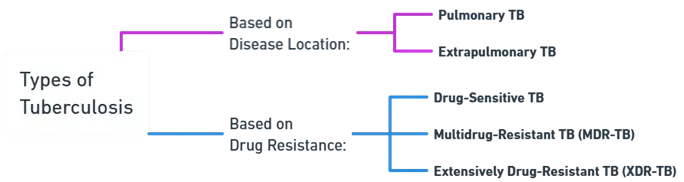
Types of Tuberculosis
-
Based on Disease Location:
- Pulmonary TB: Affects the lungs.
- Extrapulmonary TB: Affects organs other than the lungs.
-
Based on Drug Resistance:
- Drug-Sensitive TB: Responds to standard anti-TB drugs.
- Multidrug-Resistant TB (MDR-TB): Resistant to at least isoniazid and rifampicin.
- Extensively Drug-Resistant TB (XDR-TB): Resistant to isoniazid, rifampicin, any fluoroquinolone, and at least one second-line injectable drug.
Etiology of Tuberculosis
- Causative Agent: Mycobacterium tuberculosis.
- Transmission: Airborne, through inhalation of droplet nuclei from a person with active pulmonary TB.
Pathogenesis of Tuberculosis
-
Primary Infection:
- Inhalation: tuberculosis enters the lungs.
- Phagocytosis: Alveolar macrophages ingest bacteria, which survive and multiply inside macrophages.
- Formation of Granulomas: Immune response forms granulomas to contain the infection, leading to latent TB.
-
Reactivation:
- Immune Compromise: Reactivation of latent TB occurs when the immune system is weakened.
- Active TB: Bacteria multiply, causing tissue damage and symptomatic disease.
Treatment
-
Standard Regimen for Drug-Sensitive TB:
- Intensive Phase: 2 months of isoniazid, rifampicin, pyrazinamide, and ethambutol.
- Continuation Phase: 4 months of isoniazid and rifampicin.
-
MDR-TB Treatment:
- Longer Duration: 18-24 months with second-line drugs like fluoroquinolones and injectable agents (kanamycin, amikacin).
-
XDR-TB Treatment:
- Complex Regimens: Often include bedaquiline, linezolid, and other newer drugs, lasting up to 24 months or more.
Supportive Care:
- Nutritional Support: To counteract weight loss and malnutrition.
- Management of Side Effects: Regular monitoring and management of drug side effects.
- Isolation Measures: To prevent transmission until the patient is non-infectious.
Prevention of Tuberculosis:
- BCG Vaccine: Administered in infancy in endemic countries.
- Early Detection and Treatment: Active case finding, contact tracing, and treatment of latent TB.
- Infection Control: Use of personal protective equipment (PPE) and proper ventilation in healthcare settings.